Anaesthesia facility evaluation: a Whatsapp survey of hospitals in Burundi
In the Southern African Journal of Anaesthesia and Analgesia (SAJAA), April, 2021.
Sund, G. Lipnick, M, Law, T. et al.

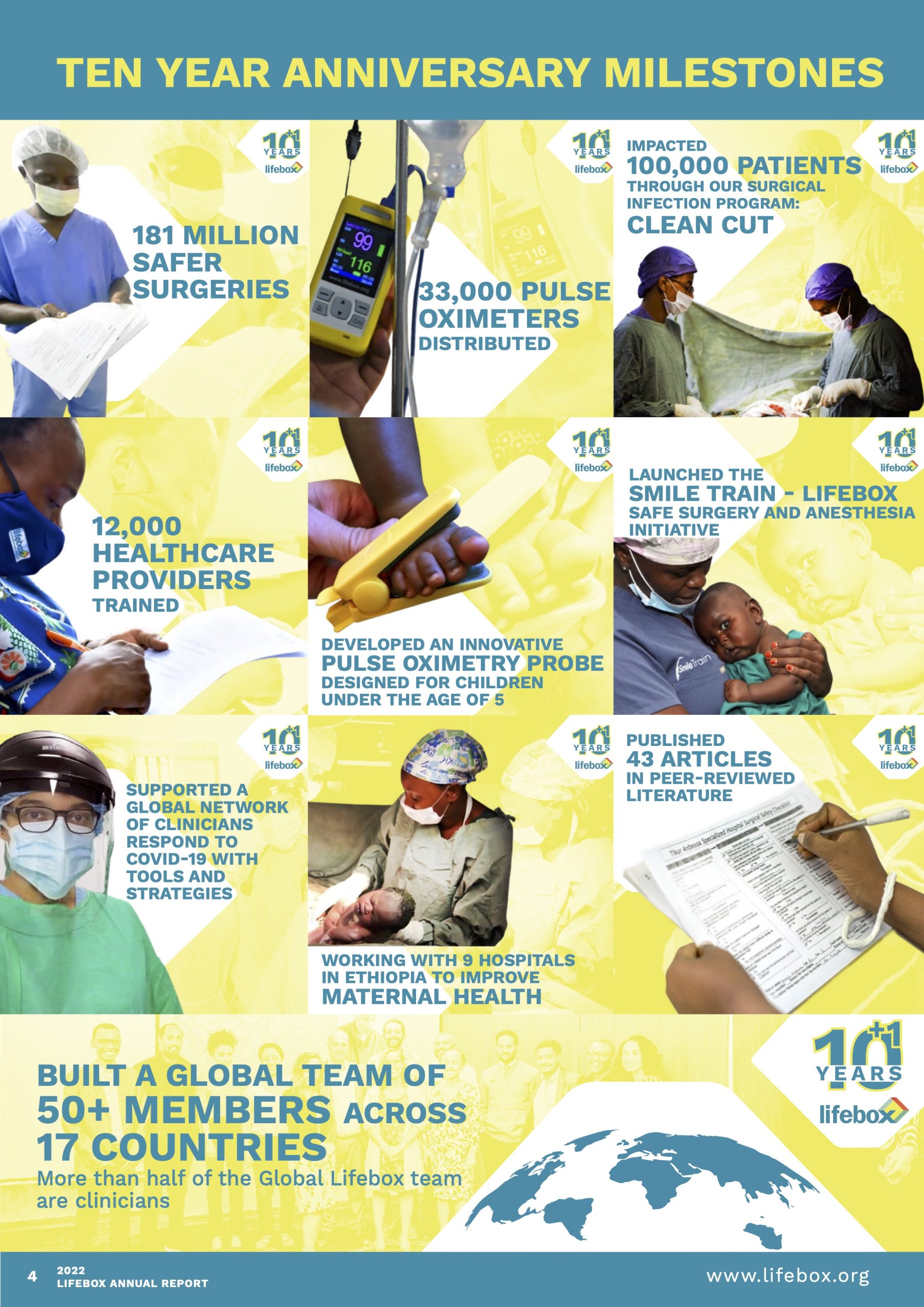
Surgery is an essential part of healthcare, enabling people to live longer and healthier lives. Surgical care can treat one third of the global burden of disease, yet surgical providers around the world face significant challenges in ensuring safe patient care. This was why Lifebox was created in 2011.
Ten years on we can point to 181 million safer surgeries through our tools, training, and partnerships. We have worked across 116 countries, trained 12,000 healthcare providers, and distributed 33,000 pulse oximeters that are essential for safe anesthesia care.
This annual report covers the first year of Lifebox’s strategic plan and focuses on our three critical areas for improving surgical patient safety – anesthesia safety, surgical teamwork, and infection reduction – from research on Lifebox’s work – including follow-up data of 3,000 patients on the lasting results of our surgical infection reduction program – to updates on Lifebox’s randomized control trial for improved maternal health.
Thank you to our supporters, partners, and donors, who have enabled Lifebox over the last decade to become a global leader in anesthesia and surgical safety. We look forward to sharing the milestones and impact of this work with you as we make surgery and anesthesia safer for every patient, every time.

Our 2021-24 Strategic Plan – Stronger Teams, Safer Surgery – puts multidisciplinary teamwork at the heart of the Lifebox approach by strengthening the professions and processes both within and beyond the operating room. The plan aims to increase the quality and impact of Lifebox programs to target the most critical moments in the end-to-end surgical patient journey.
We aim to achieve measurable improvements in the safety of surgery and anesthesia at 400 facilities in 20 countries over the next three years. Our measures of success, include:
We have also set ambitious goals for investing in staff, leadership, and innovation in the regions where we work with 80 percent of the Lifebox team, including the majority of leadership positions, based in the Global South.
This was the second year of the groundbreaking Smile Train-Lifebox Safe Surgery and Anesthesia Initiative: A multiyear program elevating the quality and safety of cleft and pediatric surgery. Through training and technological innovation, the Initiative is addressing gaps in cleft and pediatric surgical and anesthesia care – strengthening the surgical system as a whole.
Dr. Atul Gawande served as Inaugural Global Ambassador, before handing over to Professor Miliard Derbew in December 2021.

“I am absolutely honored to serve as the Global Ambassador of the Smile Train-Lifebox Safe Surgery and Anesthesia Initiative. In this role I will continue to advocate for focus and funding from governments and policymakers for interventions that work deeply on the surgical management of children.”Professor Miliard Derbew, Global Ambassador, Smile Train-Lifebox Safe Surgery and Anesthesia Initiative
We continued supporting healthcare providers with tools and resources for safe surgical, anesthesia, and COVID-19 care:
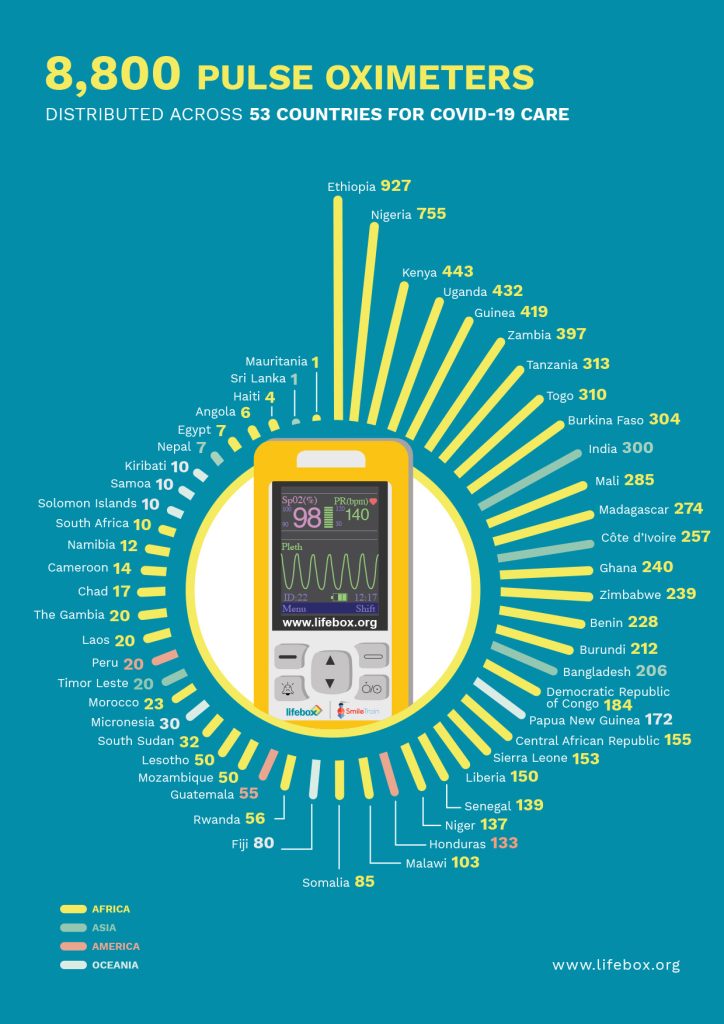 Distributing 8,800 pulse oximeters across 53 low-resource countries for the detection and management of COVID-19 patients.
Distributing 8,800 pulse oximeters across 53 low-resource countries for the detection and management of COVID-19 patients.Smile Train and Lifebox are developing a robust, affordable capnography device for use in low-resource settings. Despite being listed as an ‘essential’ safety monitoring device by the WHO-WFSA International Standards for a Safe Practice of Anesthesia, there is a lack of capnography availability throughout many LMICs. A study in Malawi found the country had only one capnograph available nationally – shared among 31 operating rooms – a 97 percent gap2.
We are working to address the capnography gap with a device designed for the intraoperative care of children. Shortlisted devices are currently being tested in the laboratory and with anesthesia providers in six countries.
We began adapting Clean Cut specifically for cleft surgeries. Alongside reducing infection, the program will address the main complications faced by cleft patients undergoing surgery, such as airway compromise or delayed bleeding. Clean Cut for Cleft will launch at two Smile Train partner hospitals in Ethiopia and one in Cote d’Ivoire. Read more.
TEAM Cleft is a new multidisciplinary workshop that brings together the three main professional groups – anesthesia providers, nurses, and surgeons – that work together as ‘Cleft teams’. The workshop focuses on improving teamwork and communication processes during emergency events, as well as routine best practices for surgical safety and will pilot in Ethiopia, Kenya, and Uganda. Read more.
Surgical site infections (SSIs) are a common and devastating complication of surgery. The Lifebox Clean Cut® program reduces infection by strengthening adherence to six key infection prevention practices.
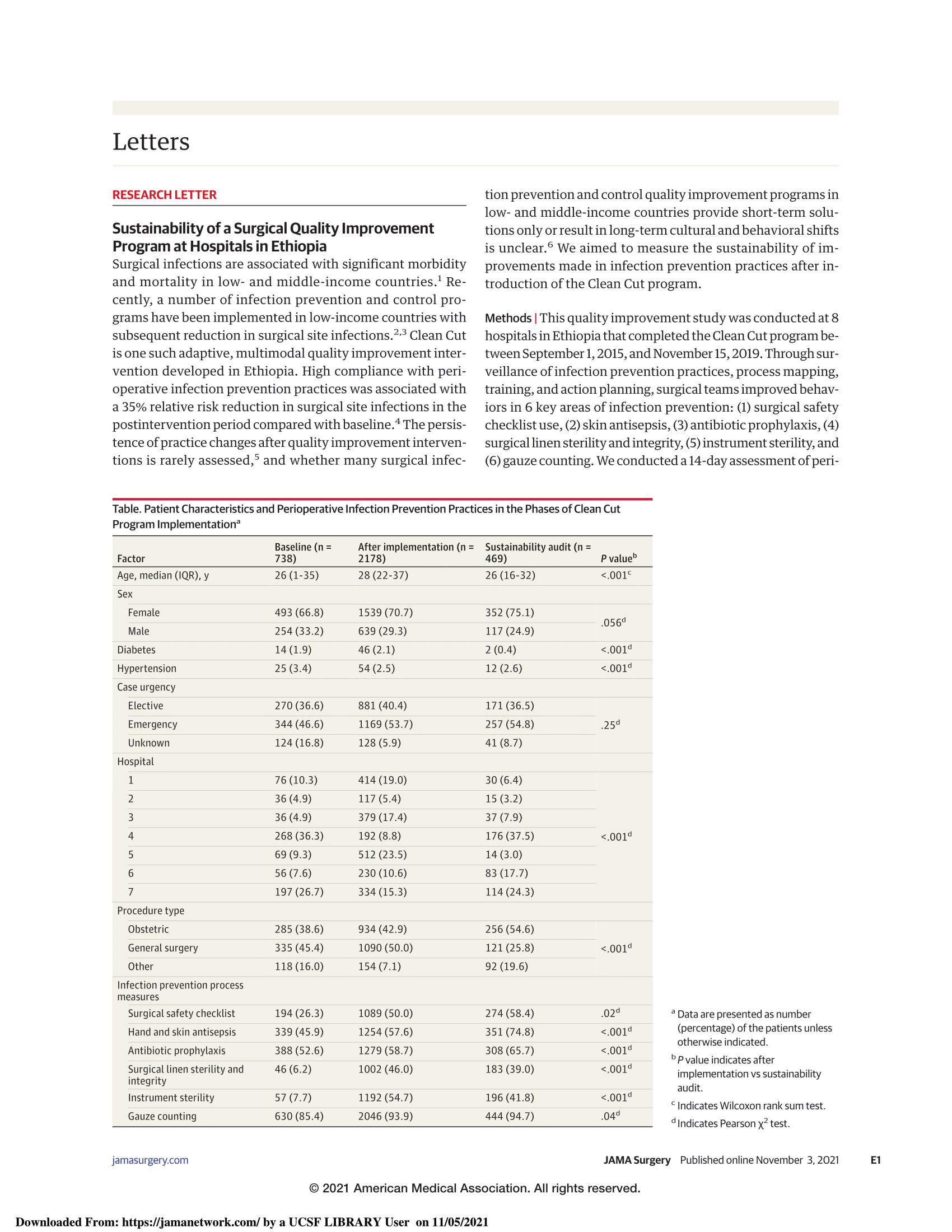
In November 2021, The Journal of the American Medical Association (JAMA) Surgery published “Sustainability of a Surgical Quality Improvement Program at Hospitals in Ethiopia” which detailed the results of a followup audit of more than 3,000 patients at seven hospitals, six to eighteen months after completion of the Clean Cut program3.
The results show that hospitals maintained improvements in compliance with all six program infection prevention standards – with compliance continuing to improve in four standards – demonstrating the lasting behavior changes achieved by Clean Cut.
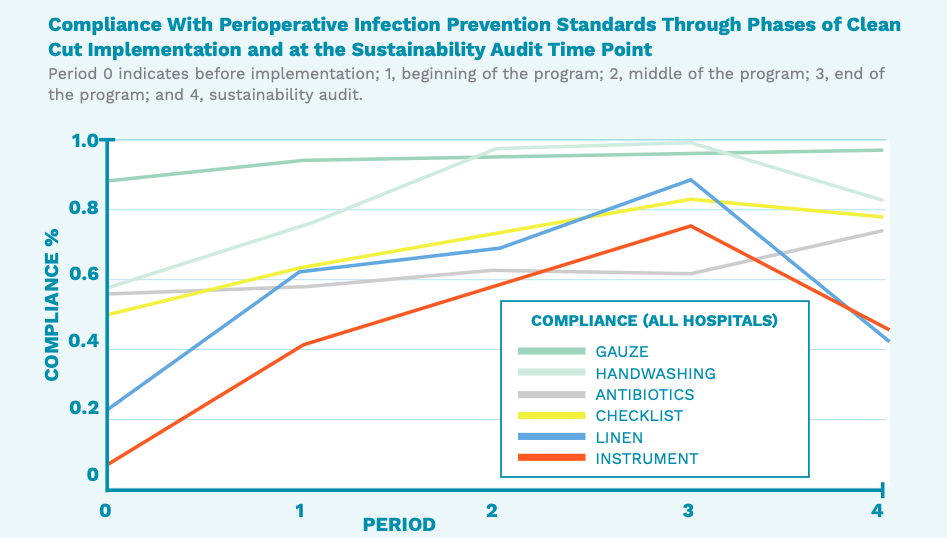
Lifebox is scaling Clean Cut to multiple sites and contexts with 25 partner hospitals in Ethiopia, India, Liberia, and Madagascar.
Cesarean section (C-section) is the most commonly performed major operation in the world, yet patients are at risk of infection. Lifebox is implementing a randomized control trial in Ethiopia to improve c-section safety by adapting our Clean Cut program. The study is being carried out at nine maternity hospitals with 4,317 patients participating in the study to date.
In Ethiopia, nine percent of patients undergoing C-sections are estimated to develop an infection. Infections and complications following C-sections are estimated to cause 15 percent of maternal deaths in the country.
This work is part of the Bill and Melinda Gates Foundation’s Grand Challenges Initiative, funded by UBS Optimus Foundation.


“Surgical site infections from C-sections are a leading cause of harm for mothers in Ethiopia. Supporting Lifebox to adapt Clean Cut will enable Lifebox and partners to drive lasting improvements in maternal health across the country and, we hope, beyond.”Dr. Tihitena Negussie, Program PI and Lifebox Global Clinical Director
Globally nurses constitute the highest number of health professionals providing care to patients and play a critical role in patient care before, during, and after surgery. In many low-resource settings, perioperative nurses face significant challenges due to hierarchical structures and organizational barriers.
A survey of perioperative nurses conducted by Lifebox in Liberia and Ethiopia found that the top five perceived training needs were: nursing-led research (72 percent); taking on leadership roles (50 percent); communication with colleagues (28 percent); monitoring the needs of critically unwell patients (28 percent); and preventing infection (22 percent).
The Perioperative Nursing Project is a new stream of work focused on building the leadership and management skills of perioperative nurses. The project will pilot in Liberia and Ethiopia.
Lifebox is driven by data to inform and shape our work. This year nine articles were published on Lifebox’s work, from program sustainability and perioperative safety, to innovations in decontamination.
In the Southern African Journal of Anaesthesia and Analgesia (SAJAA), April, 2021.
Sund, G. Lipnick, M, Law, T. et al.
In The British Medical Journal, June, 2021.
Mammo, T. Weiser, T.
In Journal of Anesthesia, August, 2021.
Miyasaka, K. Shelley, K. Takahashi, S.et al.
In Anesthesiology, October, 2021.
Hanneberg, A.
In Journal of the American Medical Association Surgery, November, 2021
Starr, N. Nofal, M. Gebeyehu, N. et al.
In Annals of Surgery,
December, 2021.
Starr, N. Capo-Chichi, N. Moore, J. Shreckengost, C. et al.
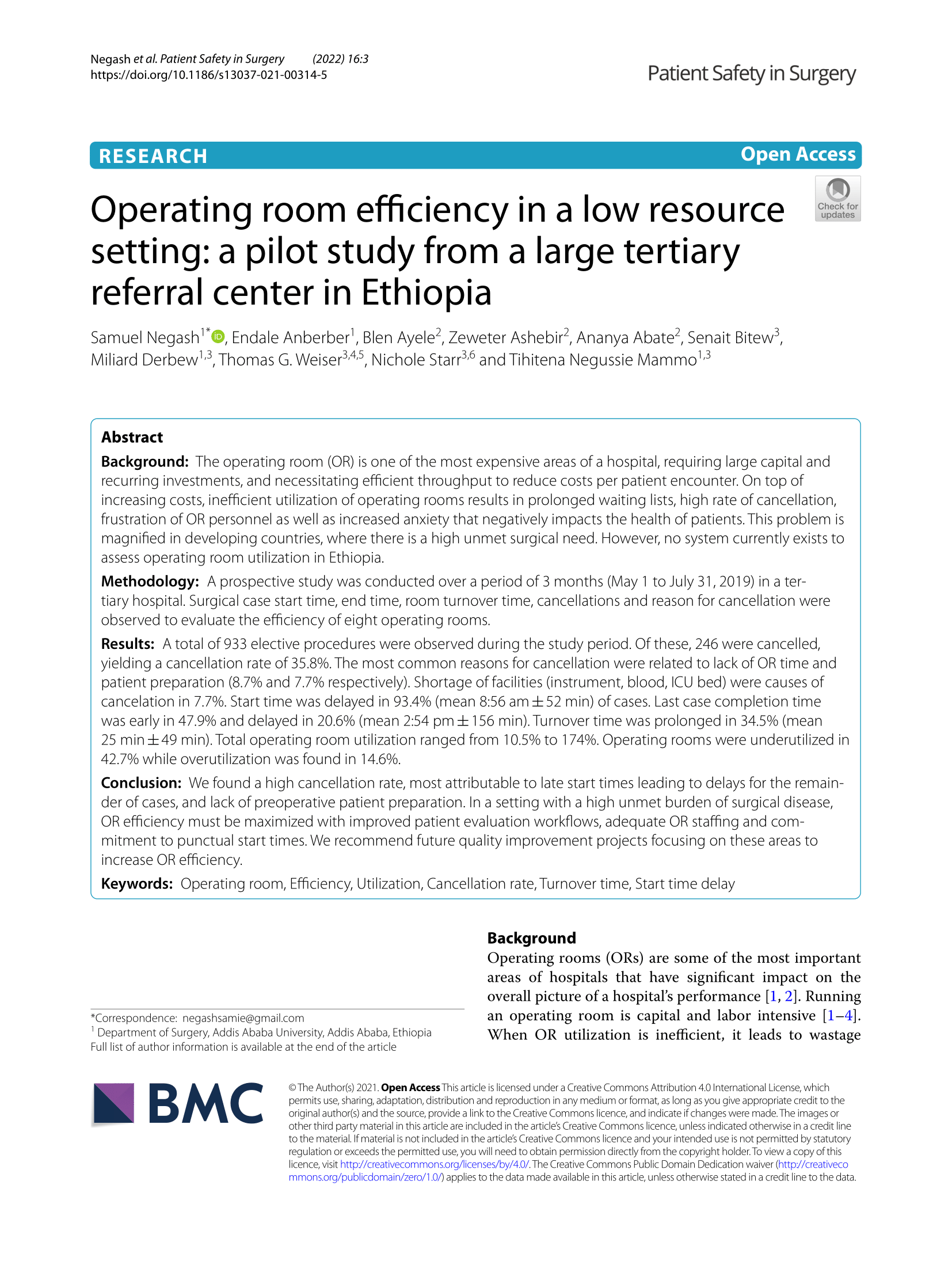
In Patient Safety in Surgery, January, 2022.
Negash, S. Anberber, E. Ayele, B. et al.
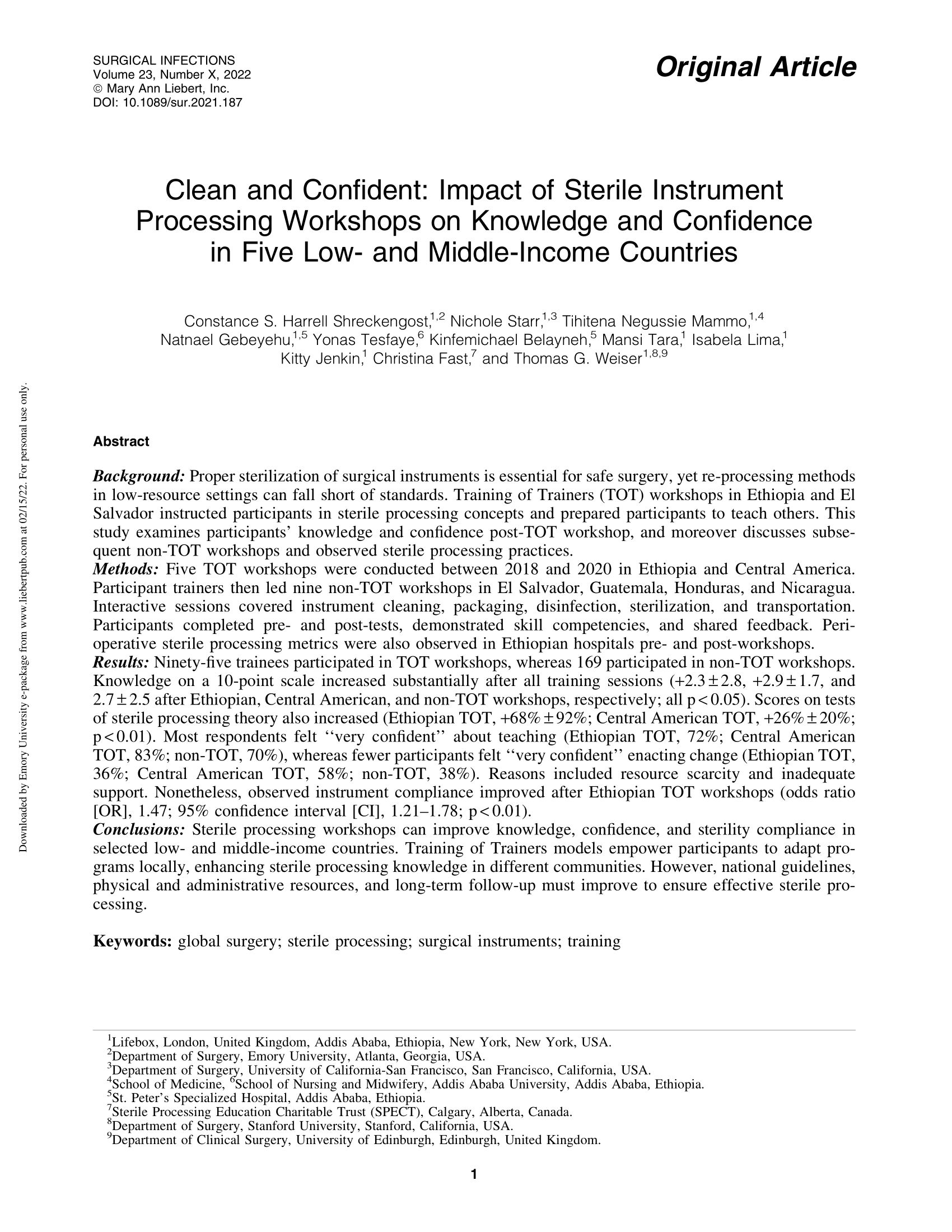
In Surgical Infections, January, 2022.
Shreckengost, C. Starr, N. Mammo, T. et al.
In New England Journal of Medicine Catalyst, February, 2022.
Starr, N. Gebeyehu, N. Gomes, A. et al.
 The study, published in SAJAA, focused on the availability of five pieces of anesthesia equipment in Burundi that are recommended by the WHO–WFSA International Standards for a Safe Practice of Anesthesia4. The study found that 89 percent of hospitals had a Lifebox pulse oximeter. While 91 percent of respondents reported the presence of an anesthesia machine, 52 percent reported that their machines were not functional or only partially functional – highlighting the critical role of pulse oximetry in providing patient monitoring during anesthesia.
The study, published in SAJAA, focused on the availability of five pieces of anesthesia equipment in Burundi that are recommended by the WHO–WFSA International Standards for a Safe Practice of Anesthesia4. The study found that 89 percent of hospitals had a Lifebox pulse oximeter. While 91 percent of respondents reported the presence of an anesthesia machine, 52 percent reported that their machines were not functional or only partially functional – highlighting the critical role of pulse oximetry in providing patient monitoring during anesthesia.
“Our study also highlights Lifebox’s impact in Burundi, with respondents from 89% of hospitals reporting the use of Lifebox pulse oximeters. Since September 2017, there have been three Lifebox workshops held in Burundi, and 116 pulse oximeters distributed. These workshops included training on maintenance and proper usage of the Lifebox pulse oximeter and how to recognise and treat hypoxia, as well as implementation of the WHO surgical safety checklist.”
Since 2017 Lifebox has partnered with the national association of anesthesia providers in Burundi, – Agora des Techniciens Supérieurs Anesthésistes Réanimateurs pour la Promotion de la Santé (ATSARPS) – to distribute 423 devices for improved anesthesia safety.
The Lifebox Global Governance Council brings together decades of clinical, research, and resource management experience to govern Lifebox’s global team and safer surgery vision. This year we welcomed a new Chair and three new members to the Council.
Lifebox co-founder – Dr. Atul Gawande – stepped down as Chair to take up the role of Assistant Administrator of the Bureau for Global Health with USAID. We are enormously grateful for Dr Gawande’s leadership and vision during our first impactful decade.
We are proud to welcome Pauline Philip as the new Lifebox Chair as well as Drs. Susana Abrego and Rob McDougall – pediatric anesthesiologists in El Salvador and Australia respectively – and Professor Salome Maswime, an obstetrician and gynecologist at the University of Cape Town.
We also want to thank Drs. Angela Enright and Isabeau Walker, two of our founding Council members who joined Dr. Iain Wilson as Emeritus Trustees. We are grateful for their commitment to Lifebox and the countless lives impacted by their work to improve anesthesia care globally.
Lifebox Global Governance Council
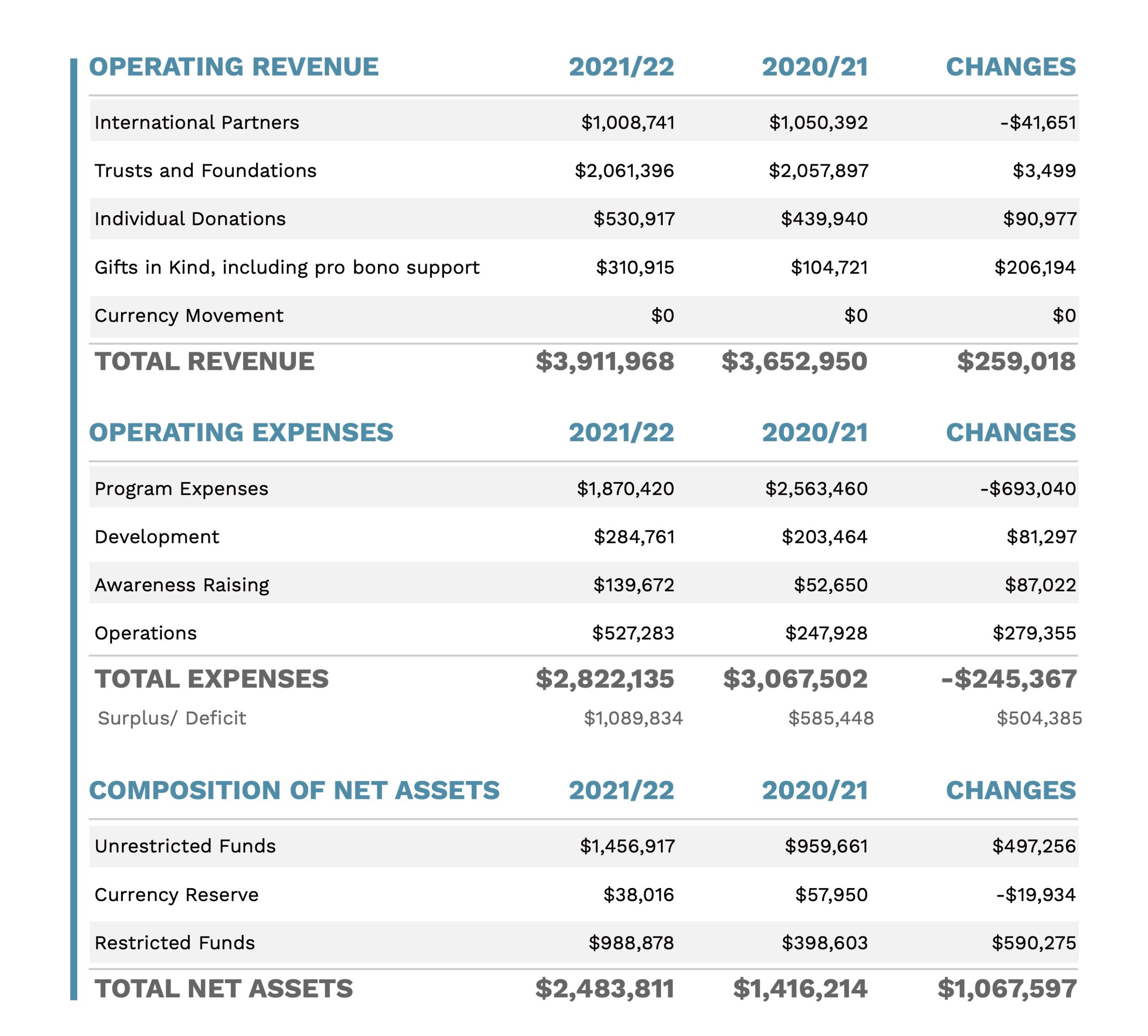
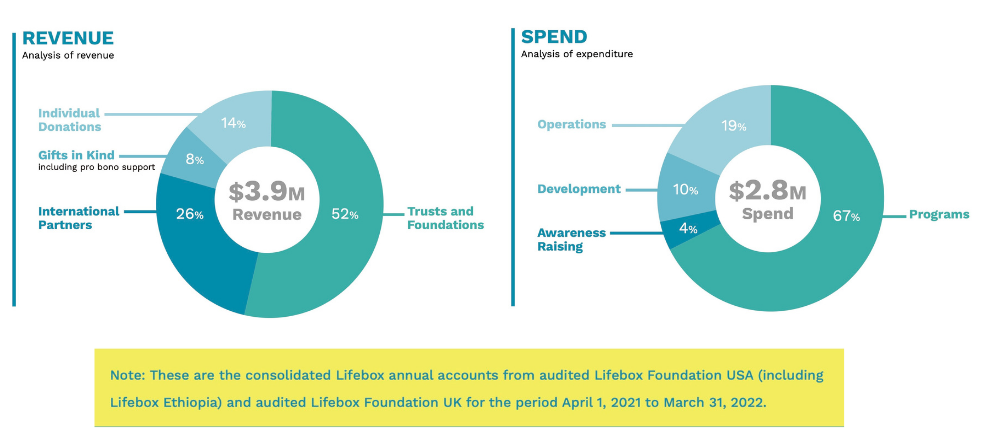
Each year Lifebox provides a global overview of its audited financial accounts by presenting the combined accounts of Lifebox Foundation UK and Lifebox Foundation USA. The combined accounts provide a full financial picture of our funding sources and how donations are being used. Our individual audited financial reports are publicly available and can be found on our website. Lifebox’s fiscal year runs from April 1 to March 31.

Our work relies on the generosity of our donors. Help equip healthcare providers around the world with essential tools and training to make surgery safer. Please donate and make a lifesaving difference today.
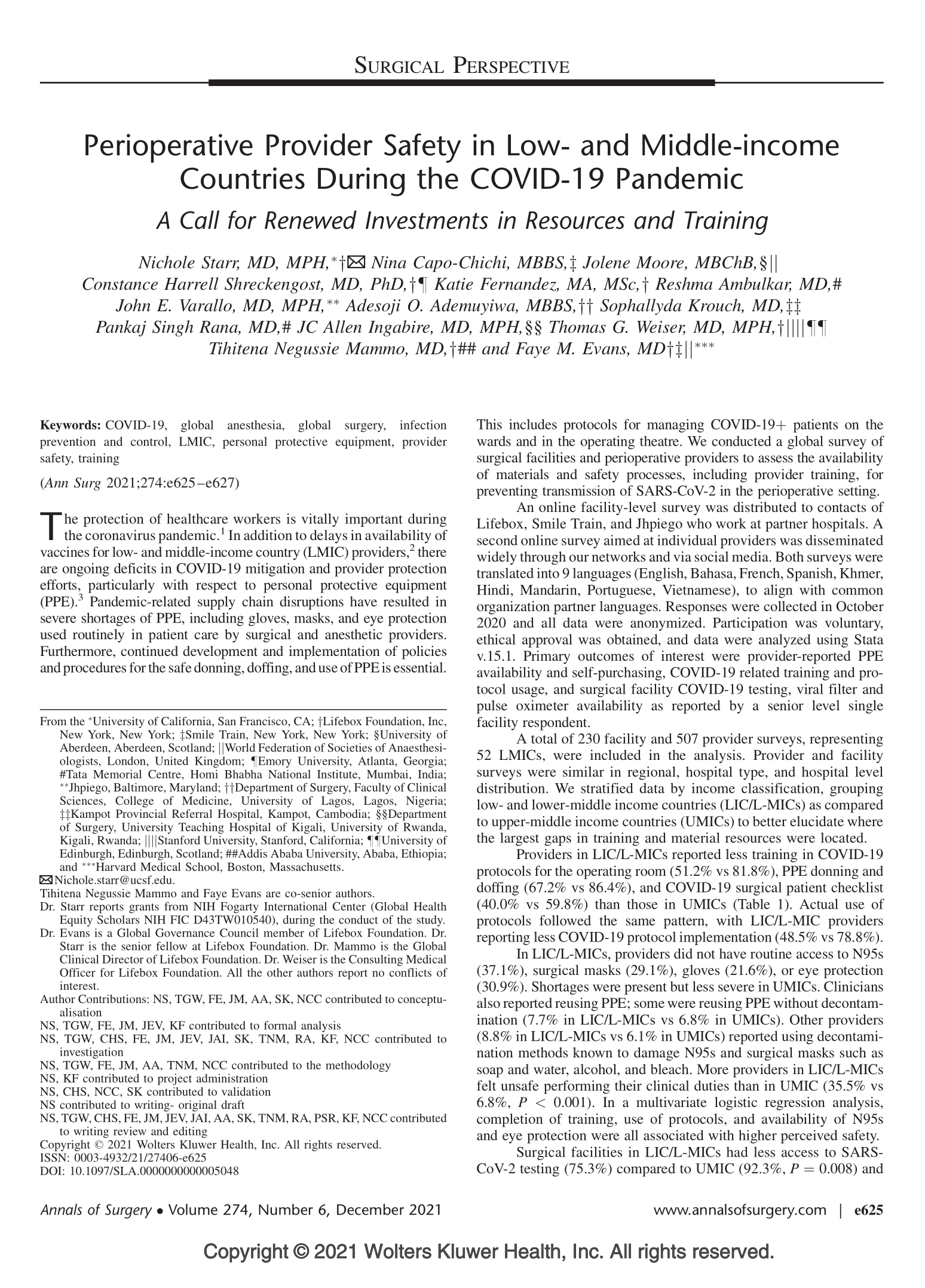
1 Starr, N. Capo-Chichi, N. Moore, J. Shreckengost, C. et al. ‘Perioperative Provider Safety in Low- and Middle-income Countries During the COVID-19 Pandemic: A Call for Renewed Investments in Resources and Training’ in Annals of Surgery Dec, 2021.
2 Jooste, R. Roberts, F. Mndolo, S. et al. Global Capnography Project (GCAP): implementation of capnography in Malawi – an international anaesthesia quality improvement project. Anaesthesia, 74: 158-166. 2019
3 Starr, N. Nofal, M. Gebeyehu, N. et al. ‘Sustainability of a Surgical Quality Improvement Program at Hospitals in Ethiopia’ in Journal of the American Medical Association Surgery, Nov, 2021
4 Sund, G. Lipnick, M, Law, T. et al. ‘Anaesthesia facility evaluation: a Whatsapp survey of hospitals in Burundi’ in Southern African Journal of Anaesthesia and Analgesia (SAJAA), April, 2021.

