Publication of the CLEAN-CS Study Protocol in 'Trials'
This protocol describes the Lifebox trial evaluating Clean Cut's ability to reduce infections following cesarean sections in Ethiopia
CLEAN-CS is a cluster-randomized stepped wedge interventional study to evaluate a multimodal, adaptive program to reduce surgical infections following cesarean delivery.
CheckList Expansion for Antisepsis and iNfection Control in Cesarean Section – CLEAN-CS:
Surgical Site infection (SSI) is a common and devastating complication of surgery, and infection rates are particularly high in low- and middle-income countries (LMICs). Cesarean section (CS) is the most commonly performed major operation in the world and patients are at risk from complications, including SSI.
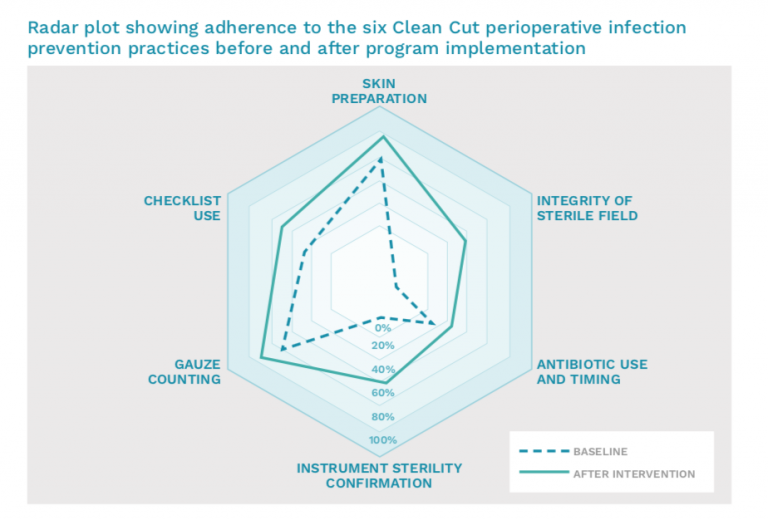
Lifebox’s Clean Cut program focuses on improving compliance with six critical surgical infection prevention standards to reduce the rate of SSIs. The Clean-CS Trial will study the impact of these six surgical infection prevention standards on patients undergoing CS. Clean-CS is a cluster-randomized stepped wedge interventional study to evaluate this multimodal, adaptive program to reduce surgical infections following cesarean delivery.
Primary Study Objective:
Secondary Objectives:
Ancillary Objectives
To assess facility readiness for and capacities to engage in quality improvement programs in surgery
The impact of the CS-tailored Clean Cut program will be tested through a stepped-wedge trial at 10 hospitals over the course of 24 months. These hospitals will start by collecting compliance information and outcomes on all patients undergoing CS prior to implementation. Over the course of 10 months, two hospitals at a time will begin implementing Clean Cut.
CS is the single most common surgical procedure performed worldwide. In Ethiopia, the majority of operations performed are considered essential surgical procedures, estimates suggest that CS accounts for 30-50% of all operations performed.
The maternal mortality rate in Ethiopia is 401 per 100,000 live births and neonatal mortality 30 per 1,000 live births. Infections and complications following CS are estimated to cause 15% of maternal deaths in the country, and the overall SSI rate following CS is estimated at 12%.
The World Health Organization recommends national CS rates of between 10-15% to save lives and improve maternal and neonatal outcomes. Population-based work indicates that CS rates of up to 19% are demonstrably related to improved maternal and neonatal survival. In Ethiopia, the national CS rate per live births was 1.9% in 2016, but rates are highly variable by region. Approximately 10.6% of births occur by CS in urban areas, compared to 0.9% of CS births in rural areas. In addition, complications are common, and gynecological and obstetric surgical interventions are associated with high rates of morbidity. Many complications are preventable, and quality improvement efforts are a high priority within the Ethiopian Federal Ministry of Health (FMOH).
Clean Cut:
Clean Cut engages all members of the surgical team and a hospital’s management to map out surgical safety processes and identify where these can be strengthened to improve adherence to six essential perioperative infection prevention practices:
The results of Clean Cut – published in the British Journal of Surgery – detailed the impact of Clean Cut in five pilot hospitals in Ethiopia. Using the outcomes of over 2,000 surgical patients, the results show a reduction in the risk of SSIs by 35%. Most importantly, for scalability across low- and middle-income countries, Clean Cut requires no major investments in new infrastructure or resources.
“Clean Cut was able to leverage teamwork and multidisciplinary action to dramatically improve compliance with essential perioperative infection prevention standards. This improvement in adherence to such critical standards resulted in profound reductions in postoperative infections. The Grand Challenge Initiative allows for a rigorous study of Clean Cut and its impact on the safety of C-sections.”Dr. Thomas Weiser, Program PI, Consulting Medical Officer of Lifebox and an Associate Professor of Surgery at Stanford University.
This protocol describes the Lifebox trial evaluating Clean Cut's ability to reduce infections following cesarean sections in Ethiopia




Dr. Thomas Weiser is a general and trauma surgeon, a surgical intensivist, and an associate professor of Surgery at Stanford University Medical Center and currently serves as Lifebox’s Consulting Medical Officer.






Dr. Tihitena Negussie is an associate professor and a consultant general and pediatric surgeon at Addis Ababa University and is currently serving as Lifebox’s Global Clinical Director.






Dr. Mekdes Daba is assistant professor of obstetrics and gynecology at St Paul’s Hospital Millennium Medical College in Ethiopia and the current president of the Ethiopian Society of Obstetricians and Gynecologists.






Professor Salome Maswime is an obstetrician and gynecologist and professor and Head of the Global Surgery Division at the University of Cape Town. Professor Maswime is a World Economic Forum Young Scientist; Next Einstein Fellow, and President of the South African Clinician Scientists Society.






Dr. Stephen Rulisa is professor of obstetrics & gynecology at the School of Medicine & Pharmacy, University of Rwanda.






Dr. Meseret Zelalem is a pediatrician and serves as Director for maternal, child health, youth adolescent and nutrition Directorate at the Federal Ministry of Health of Ethiopia. Prior to this Dr. Zelalem served as assistant professor of pediatrics and child health at University of Gondar.
Partners:
Ethiopian Society of Obstetricians and Gynecologists
Ethiopian Federal Ministry of Health
Ariadne Labs
This study is part of the Bill & Melinda Gates Foundation Grand Challenges initiative, funded by UBS Optimus Foundation.



