But it could be so much more
“We have a couple of monitors from the US. Lovely, lovely multi-parameter monitors – but they only work with a battery. And they didn’t send the battery.”
“People send things with the best of intentions, but they’re not thinking about where these things are going to be used,” explained Dr Eva Manciles-Robert, when she visited the Lifebox office yesterday to confirm plans for the workshop she’ll be running in April at the Connaught Hospital in Freetown, Sierra Leone.

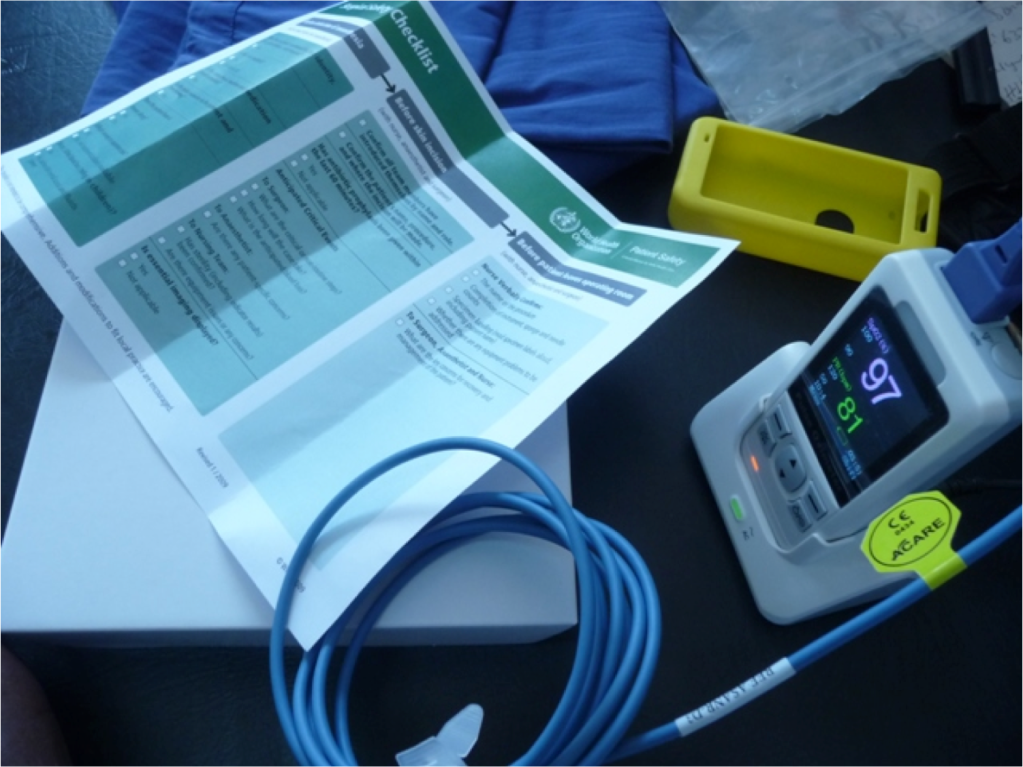
Dr Eva Manciles-Robert visits London and demonstrates the pulse oximeter (in colour-coordinated style)
In Sierra Leone, where Dr Manciles-Robert returned to practice in 2007, you need equipment that is fit for purpose. Like the Lifebox oximeter.
It’s high quality but it does a very specific job, for a very specific environment.
For instance – in a low-resource setting, the operating room will likely have a concrete floor, and no engineer to fix broken equipment. So the Lifebox oximeter is robust enough that you can drop it from a metre’s height off the table without immediate consignment to the equipment graveyard.
The electricity supply will almost certainly be fickle, so it runs off a rechargeable battery that can be powered up when mains power is available, and will keep a patient safely monitored throughout an operation even when the power inevitably fails.
The majority of anaesthesia providers will have between six months and two years of training before heading out to rural facilities where they will be the only person qualified to deliver anaesthesia for miles around. So the Lifebox oximeter is intuitive, with a basic interface and large screen. And the education materials come in six different languages.
There are only two medical anaesthetists in the entire country of Sierra Leone, as well as 60 nurse anaesthetists. (“Sixty more than there were just after the war,” Dr Manciels-Robert reminded us.) They are responsible for the anaesthesia care of 6 million people. And they handle everything.
So the Lifebox workshop that Dr Manciles-Robert is leading will make an enormous difference. Over two days, nurse anaesthetists will learn about pulse oximetry and the WHO Surgical Safety Checklist.
Thanks to our donors Dr Manciles-Robert will be able to distribute 36 oximeters, ensuring that every operating room in the country is equipped. Surgeons and anaesthesia providers in the provinces will be able to do more complex cases, safely, rather than sending patients hundreds of miles to over-crowded, under-resourced main hospitals.
“When I went back I was in awe of my colleagues,” said Dr Manciles-Robert, who trained in Ireland. “In Sierra Leone, you go back to medicine as medicine once was. You depend on your finger, eyes, nose. But it could be so much more.”
We’ll keep you updated on how it goes.