Serious questions and serious answers – #BMJLifebox week two
The best thing about introductions are the questions you get back in return – after all, the surgical safety crisis is going to improve through dialogue, not monologue! – and when they have a question, the readership of the British Medical Journal is certainly not afraid to ask.

Anaesthetic officers at Kappchorwa Hospital, Uganda, with a BMJ pulse oximeter
During last year’s appeal for Lifebox, we got some really important ones.
“Is a $250/£160 pulse oximeter really necessary when you can buy cheaper online?”
“Can you prove the impact of pulse oximetry in the operating theatre?”
Yes and yes and yes, with a conviction that isn’t just a case of high mission-fever; the rationale behind our answers is fundamental to the development of Lifebox, and we were glad to be able to discuss it further in the BMJ this week.
Atul Gawande, surgeon, author and Lifebox Chair, spoke about these issues and more in conversation with journalist Jane Feinmann.
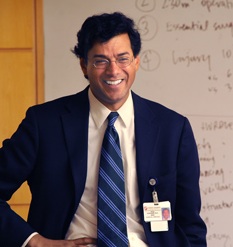
Dr Atul Gawande
The interview is in the journal this week, with an extended version online. You can also catch a podcast of Atul in conversation for that authentic dialogue experience!
So there’s the scholarship, the methodology, the high-level view. But it’s not a different conversation in the field. They’re saying exactly the same from the front line – only the cases are personal, and the stories are heart-breaking.
“Can I ask your advice doctor?” Tom Bashford, a volunteer anaesthetist working at a hospital in Ethiopia recalls being asked, on his 10-month VSO placement. “The recovery nurse who I had been teaching looked puzzled. “I have been asked by some of my colleagues on the wards how to wake up patients who have not recovered from their anaesthetic after one or two days. What do you suggest?”

Dr Tom Bashford at Yekatit 12 Hospital
(c) VSO/Ben Langdon
“My heart sank; all of the drugs we were using for anaesthesia should have cleared within hours, and a patient who was still asleep after two days was more likely to have suffered some other untoward event. After a few months of working in Ethiopia, I had a near certain guess as to the cause.”
Click over to the BMJ blog for the rest of the piece – it’s a conversation no healthcare worker should have to have, and no patient, or family; but it’s part of the reality of unsafe surgery in low-resource settings. It shouldn’t be, and we’re working to change things. Together, we can make a difference. Let’s talk.

